Tuberculosis TB: Symptoms, Causes, & Treatment Understanding Tuberculosis (TB): Symptoms, Causes, and Solutions
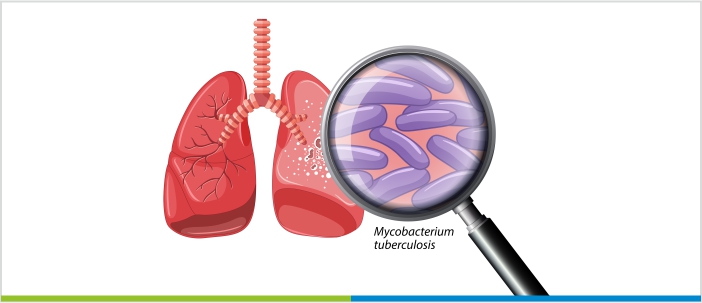
Tuberculosis (TB) is an infectious disease caused by the bacterium Mycobacterium tuberculosis. These bacteria primarily target the lungs and other body parts. The disease traces back thousands of years and has caused havoc across continents, leading to widespread morbidity and mortality. Though there are major medical advancements and efforts to combat the disease, tuberculosis (TB) continues to be a major public health threat.
It is important to understand the causes and symptoms in addition to the importance of timely medical intervention. It can significantly reduce its spread and mortality rate. Moreover, raising awareness and implementing robust public health strategies are necessary steps towards controlling and eliminating Tuberculosis (TB).
Symptoms of Tuberculosis (TB)
Mycobacterium tuberculosis, the bacteria that causes tuberculosis, can infect certain people even when they show no symptoms. These bacteria survive and multiply in the lungs, causing the infection. The symptoms of the Tuberculosis (TB) disease vary depending on the stage of the condition, as mentioned below:
Primary Tuberculosis (TB) Infection
This is the first stage of Tuberculosis (TB) infection, where the immune system cells find and capture the bacteria while destroying them. But sometimes, the captured bacteria might survive and then multiply. During the first stage, most people do not have any symptoms, while some might have flu-like symptoms such as:
- Low fever
- Tiredness
- Cough
Latent Tuberculosis (TB) Infection
This is the second stage of infection, in which the immune system builds a wall around the lung tissue with the TB bacteria inside. Hence, the bacteria can do no harm to the body, which is why this stage does not show any symptoms.
Active TB Infection
When the immune system cannot hold the bacteria inside the wall created by them, the bacteria get out of control and cause infection throughout the lungs and other body parts. This might happen immediately after the primary stage, or it might happen after the latent stage. Symptoms of active Tuberculosis (TB) infection include:
- Cough
- Chest pain
- Not feeling well
- Fever with chills
- Coughing up blood or mucus
- Night sweats
- Weight loss
- Tiredness
Causes and Risk Factors of Tuberculosis (TB)
Tuberculosis is caused by a bacteria called Mycobacterium tuberculosis, which can affect the lungs and voice box and spread to other parts of the body. These diseases are mainly spread when a healthy person is in contact with the infected person for a long time. The immune system may contain the bacteria, leading to a latent TB infection, or fail to do so, allowing the bacteria to multiply and cause active TB disease, damaging lung tissue and possibly spreading to other organs.
Here are some of the risk factors for TB:
- Compromised Immune System: Individuals with weakened immune systems due to conditions like HIV/AIDS or treatments like chemotherapy are at a significantly higher risk as their bodies are less capable of fighting off TB bacteria.
- Contact with TB Patients: Regular close contact with someone who has active TB significantly increases the risk of contracting the infection due to prolonged exposure to the bacteria.
- Living Conditions and Overcrowding: People living in overcrowded conditions, such as shelters or prisons, face a higher risk because the close quarters facilitate the spread of TB bacteria.
- Socioeconomic Factors: Poverty, malnutrition, and lack of access to medical care can weaken the immune system, making individuals more susceptible to developing TB if exposed.
- Substance Abuse: Tobacco and alcohol use can weaken the lung’s ability to fight infections and are associated with a higher risk of TB.
- Healthcare Work: Healthcare workers are at an increased risk due to more frequent exposure to patients with active TB.
Airborne droplets contaminated with tuberculosis bacteria spread the disease. Once in the air, anyone in the vicinity can breathe in these droplets. A tuberculosis patient may spread bacteria through snoring, coughing, talking, and singing.
Certain populations are more vulnerable to TB due to factors like compromised healthcare access, living in crowded conditions, and underlying health issues. These conditions make it difficult to prevent exposure to TB and to access timely, effective treatment, thereby increasing the incidence of TB within these communities.
How is Tuberculosis Diagnosed?
Here’s how tuberculosis is diagnosed:
Mantoux Tuberculin Skin Test:
- A small amount of tuberculin is injected under the skin.
- The injection site is observed after 48-72 hours for any reaction, indicating TB exposure.
Blood Tests (Interferon Gamma Release Assays – IGRAs):
- Measure the immune system’s response to TB bacteria.
- Includes tests like QuantiFERON-TB Gold Plus and T-SPOT.TB.
Note: Useful especially for those who have received the BCG vaccine or where a skin test might not be practical.
Chest X-rays:
- Used to detect active TB disease in the lungs.
- Provides visual evidence of infection, such as abnormal shadows or patterns.
Also, doctors recommend sputum tests, in which the healthcare provider may take a sample of mucus that comes up while coughing (sputum). If a person has active TB, a lab test can easily detect the infection. Though it tells if a person has TB bacteria, it might also show bacteria with similar features.
Other lab tests may include –
- Urine test (urology test)
- Breath test
- Procedure to remove sputum from lungs with a tube
- Tests of the fluid around the spine and brain, called cerebrospinal fluid
How is Tuberculosis Treated?
The treatment of the TB bacteria depends on the type of TB. If a person has a latent TB infection, doctors might start with drug treatment. This is the best treatment plan for patients with HIV and AIDS or other factors that increase the risk of TB infection.
- It involves a standard drug regimen, including isoniazid, rifampicin, ethambutol, and pyrazinamide. The treatment must be at least six months to ensure the eradication of TB bacteria and prevent drug resistance.
- Treatment of drug-resistant TB strains, multidrug-resistant TB (MDR-TB), and extended drug-resistant TB (XDR-TB) might take up to 24 months or longer, and are costly and sometimes ineffective due to the severity of the condition.
- However, there have been some new advancements in TB treatment, with the development of new vaccines and novel therapeutic drugs to improve treatment efficacy. Also, research is putting efforts into biomarkers for faster diagnosis and personalized medicine approaches.
- Moreover, their efforts are aimed at reducing treatment duration, combating drug-resistant strains, and customizing therapy to individual needs and the type of TB.
- Tuberculosis is a contagious bacterial disease that is transmitted to people who stay in contact with infected people for a longer period. Sometimes, the disease does not show any symptoms, and when they do, the severity of the disease increases, making it challenging to treat appropriately.
- Hence, early detection, treatment, and preventive measures are crucial in combating tuberculosis (TB). Timely intervention can prevent the spread and severity of TB. If a person experiences coughing, heavy breathing, spine pain, or any other symptoms that might indicate TB, it is important to seek medical attention.
